Wednesday, April 17, 2024 | | 6:30pm | - | 9:00pm | Open Skating Cheap-Skate Night | $9.50* |
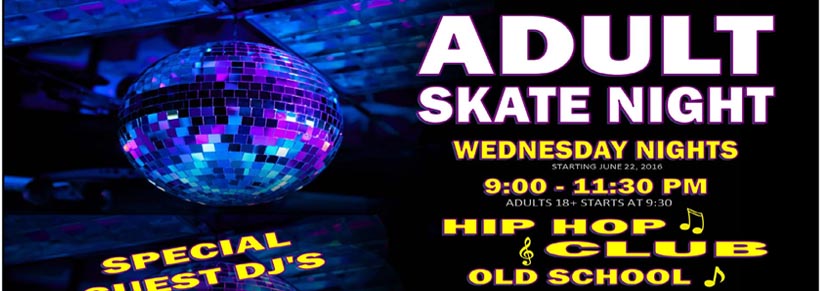
| 9:00pm | - | 11:30pm | Adult Skate Night (18 & Over) | $14.00 |
|
|
|
Thursday, April 18, 2024 | | Available for Private Parties |
|
|
|
Friday, April 19, 2024 | | 3:30pm | - | 5:30pm | After School Skate (Open Skating) | 9.50* |
| 7:00pm | - | 9:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 9:00pm | - | 11:30pm | Open Public Skating | 12.50* |
|
|
|
Saturday, April 20, 2024 | | 11:15am | - | 1:00pm | Jr. Session Open Skating 10 yo & Younger & Parents) | 9.50* |
| This is an open public skate for kids 10 years old and younger and their parents. |
|
| 1:00pm | - | 3:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 2:30pm | - | 5:00pm | Open Public Skating | 12.50* |
| 7:00pm | - | 9:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 9:00pm | - | 11:30pm | Open Public Skating | 12.50* |
|
|
|
Sunday, April 21, 2024 | | 1:00pm | - | 3:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 2:30pm | - | 5:00pm | Open Public Skating | 12.50* |
| 6:30pm | - | 9:30pm | Family Night Open Public Skating | 32.00* |
| Family Rate Available $31.00 plus skate rental. Includes up to 5 skaters. Single admission $12.00 plus skate rental. |
|
|
|
|
Monday, April 22, 2024 | | 6:30pm | - | 9:30pm | Open Public Skating | $12.50* |
|
|
|
Tuesday, April 23, 2024 | | Available for Private Parties |
|
|
|
Wednesday, April 24, 2024 | | 6:30pm | - | 9:00pm | Open Skating Cheap-Skate Night | $9.50* |
| 9:00pm | - | 11:30pm | Adult Skate Night (18 & Over) | $14.00 |
|
|
|
Thursday, April 25, 2024 | | Available for Private Parties |
|
|
|
Friday, April 26, 2024 | | 3:30pm | - | 5:30pm | After School Skate (Open Skating) | 9.50* |
| 7:00pm | - | 9:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 9:00pm | - | 11:30pm | Open Public Skating | 12.50* |
|
|
|
Saturday, April 27, 2024 | | 11:15am | - | 1:00pm | Jr. Session Open Skating 10 yo & Younger & Parents) | 9.50* |
| This is an open public skate for kids 10 years old and younger and their parents. |
|
| 1:00pm | - | 3:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 2:30pm | - | 5:00pm | Open Public Skating | 12.50* |
| 7:00pm | - | 9:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 9:00pm | - | 11:30pm | Open Public Skating | 12.50* |
|
|
|
Sunday, April 28, 2024 | | 1:00pm | - | 3:30pm | Open Public Skating | 12.50* |
| Double overlapping session. Skate both sessions for an additional $4.00. |
|
| 2:30pm | - | 5:00pm | Open Public Skating | 12.50* |
| 6:30pm | - | 9:30pm | Family Night Open Public Skating | 32.00* |
| Family Rate Available $31.00 plus skate rental. Includes up to 5 skaters. Single admission $12.00 plus skate rental. |
|
|
|
|
Monday, April 29, 2024 | | 6:30pm | - | 9:30pm | Open Public Skating | $12.50* |
|
|
|
Tuesday, April 30, 2024 | | Available for Private Parties |
|
|
|
Quad Skate Rental . . . . . $3.50 Extra Per Person
Inline Skate Rental . . . . . . .$4.50 Extra Per Person
Stay Over to Next Overlapping Session . . . $4.00